All About Psychology Newsletter
Why Do We Feel Bad When Our Beliefs Don’t Match Our Actions? Morons, Imbeciles and Idiots. The Association Method. Sundowning.
A very warm welcome to the latest edition of the All About Psychology newsletter—the official newsletter of All-About-Psychology.com, a website providing comprehensive information and resources for psychology students and educators since 2008.
Why Do We Feel Bad When Our Beliefs Don’t Match Our Actions? Blame 'Cognitive Dissonance'
Discover the Psychology Behind Everyday Inner Conflicts.
Have you ever caught yourself acting in a way that doesn’t align with your beliefs and felt that uncomfortable mental tug-of-war? That’s the fascinating phenomenon of cognitive dissonance at play! Explore why we feel uneasy when our actions don’t match our values, how our minds creatively resolve this discomfort, and how this psychological quirk can even inspire positive change. From classic experiments to everyday scenarios like recycling dilemmas, this insightful article by behavioral scientist, Dr. Kim M Caudwell reveals how cognitive dissonance shapes our behavior in surprising ways.
Read the article in full here.
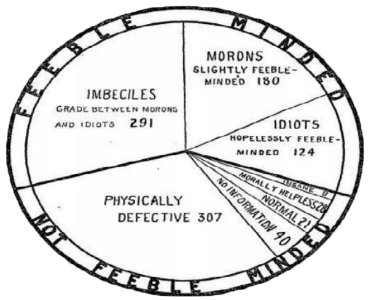
Morons, Imbeciles and Idiots
Did You Know?
During the 1910 annual meeting of the American Association for the Study of the Feeble-Minded, psychologist Henry H. Goddard proposed adopting the terms moron, imbecile, and idiot as distinct classifications of mental deficiency.
Now pejorative terms no longer employed in a psychological context, moron, imbecile, and idiot were standard definitions within the field of 'mental retardation' for many years.
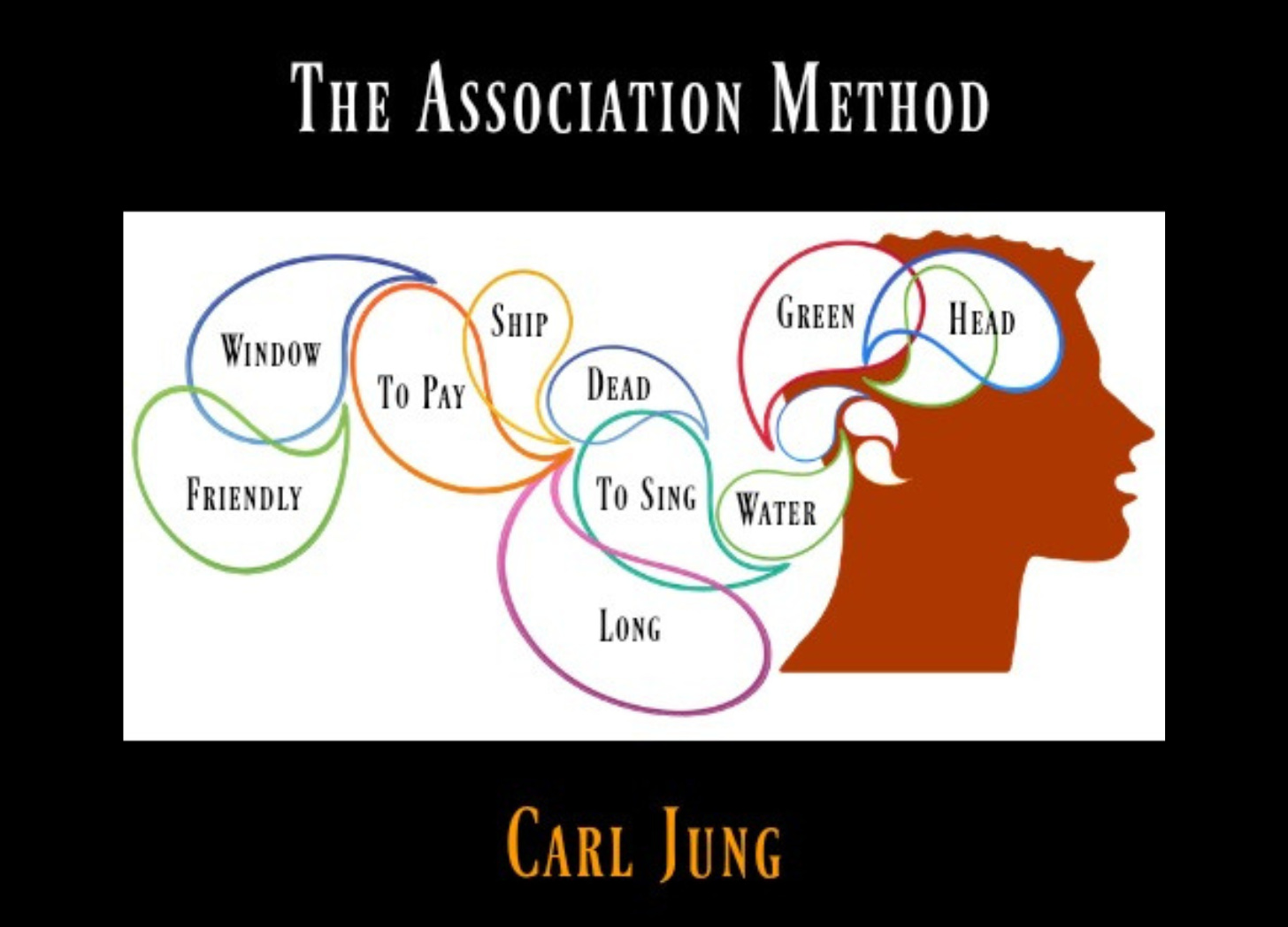
Psychology Classic
Originally published in the Collected Papers on Analytical Psychology in 1916, The Association Method was the first of three lectures Carl Jung delivered at Clark University in September, 1909. You can read the article version of The Association Method in full for free via the following link.
Psychology Q&A
Question submitted to the All About Psychology Q&A page, followed by a submitted answer.
What are the symptoms of Sundowning?
Sundowning, also known as sundown syndrome, refers to a phenomenon where individuals with certain cognitive conditions, such as dementia or Alzheimer's disease, experience worsening symptoms of confusion, agitation, and restlessness during the late afternoon and evening hours. This condition can be distressing for both the individuals affected and their caregivers. The following information addresses the symptoms of sundowning, its potential causes, and strategies for managing this challenging behavior.
Symptoms of Sundowning:
Agitation and Restlessness: One of the hallmark symptoms of sundowning is increased agitation and restlessness, which can manifest as pacing, fidgeting, or agitation.
Confusion and Disorientation: Individuals experiencing sundowning may become more confused or disoriented, having difficulty recognizing familiar surroundings or people.
Anxiety and Fear: Sundowning can also trigger feelings of anxiety or fear in affected individuals, leading to increased agitation and distress.
Aggression: In some cases, sundowning may result in aggressive behaviors, such as verbal or physical outbursts, which can pose safety concerns for both the individual and their caregivers.
Hallucinations or Delusions: Some individuals may experience hallucinations or delusions during episodes of sundowning, further contributing to their distress and confusion.
Causes of Sundowning:
While the exact causes of sundowning are not fully understood, several factors may contribute to its onset and exacerbation:
Circadian Rhythm Disruption: Disruption of the body's internal clock, known as the circadian rhythm, may play a role in sundowning. Changes in light exposure and melatonin production during the evening hours can affect sleep-wake cycles and contribute to increased agitation and confusion.
Sensory Overload: Overstimulation from noise, light, or other sensory inputs in the late afternoon and evening hours may overwhelm individuals with cognitive impairments, exacerbating symptoms of sundowning.
Fatigue and Exhaustion: Fatigue and exhaustion from the activities of the day can worsen symptoms of cognitive decline, leading to increased confusion and agitation during the evening hours.
Medication Side Effects: Certain medications commonly prescribed for cognitive conditions may have side effects that worsen symptoms of sundowning, such as increased agitation or confusion.
Management Strategies for Sundowning:
While sundowning can be challenging to manage, there are strategies that caregivers can employ to help alleviate symptoms and improve the overall well-being of individuals affected:
Establish a Routine: Maintaining a consistent daily routine can help regulate sleep-wake cycles and reduce the risk of sundowning episodes. Ensure regular mealtimes, bedtime routines, and activities throughout the day.
Create a Calming Environment: Minimize sensory stimuli in the late afternoon and evening hours by dimming lights, reducing noise, and creating a calm and soothing environment.
Promote Relaxation Techniques: Encourage relaxation techniques such as deep breathing exercises, gentle music, or aromatherapy to help individuals relax and unwind in the evening.
Monitor Medication: Work closely with healthcare professionals to monitor medication regimens and adjust doses if necessary to minimize side effects that may exacerbate sundowning symptoms.
Engage in Meaningful Activities: Encourage participation in activities that promote cognitive stimulation and social engagement during the day to reduce boredom and restlessness in the evening.
Sundowning is a complex phenomenon characterized by worsening symptoms of confusion, agitation, and restlessness during the late afternoon and evening hours. While the exact causes of sundowning remain elusive, understanding its symptoms and potential triggers is essential for effective management and support. By implementing strategies to promote a calming environment, establish a consistent routine, and address underlying factors contributing to sundowning, caregivers can help improve the quality of life for individuals affected by this challenging condition.
Psychology Q & A is open to everyone and is designed as a space for those with an interest in psychology to both give and receive help. So, if you have a psychology-related question, feel free to ask! And if you believe you can answer any of the questions posted, I encourage you to share your insights. Please note that any content generated by psychology Q & A is provided for informational purposes only. It does not signify that I endorse the material provided or the views expressed. None of the information within psychology Q & A should be considered a substitute for professional psychological, psychiatric or medical advice, diagnosis, or treatment.
With the holiday season around the corner, don't forget to visit the All About Psychology Amazon Store to check out an awesome collection of psychology books, gifts and T-shirts. Sales help support All-About-Psychology.Com, a website providing free and comprehensive information and resources for psychology students and educators since 2008.
Thanks for Reading
That's it for this newsletter, hope you found it interesting. If you’re celebrating Thanksgiving on Thursday, I hope you have a wonderful time with your friends and family. As for the day after, I’ll leave you with this!
Stay in the know! The All About Psychology newsletter is your go-to source for all things psychology. Subscribe today and instantly receive my bestselling Psychology Student Guide right in your inbox.
Upgrade to a paid subscription and also get the eBook version of my latest book Psychology Q & A: Great Answers to Fascinating Psychology Questions, as well as regular psychology book giveaways and other exclusive benefits.